Features & Benefits
- Relaxes muscle spasms, muscle cramps, strain and pain
- Decreases axial loading Increases disc height
- Advanced tubeless air cell design for narrow fit
- Can be worn discreetly under clothing
- Assists individuals with strenuous jobs
- Helps maintain proper posture (Improper posture places the upper body weight on the discs that causes back pain)
- Very lightweight and comfortable
- Made of 100% highly durable cotton
- Machine Washable
-
Simple to use
Principle of Operation
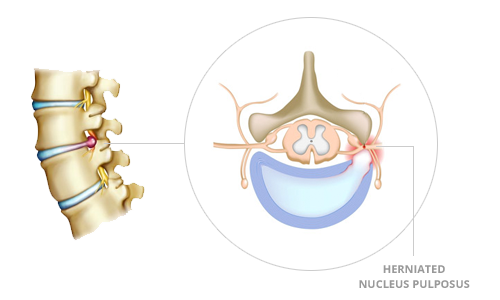
Before treatment
The herniated or bulging intervertebral disc or herniated nucleus pulposus applies pressures on the nerve root, causing pain.
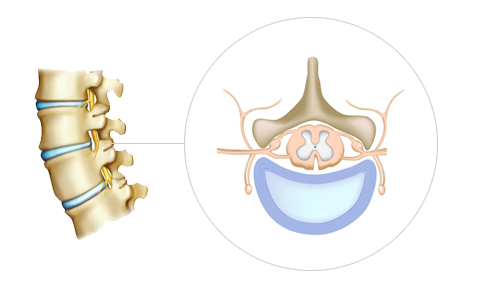
After treatment
DDS Neck and Back Braces help resume the appropriate position of the intervertebral disc or nucleus pulposus by increasing the intervertebral space thereby reducing the pressure between lumbar/cervical vertebrae.
DDS Distractive Force
Not all back braces are created equally, especially if spinal distraction/decompression is desired. Decompression is the act of external forces separating the spine in an effort to allow discs and other connective tissues to move off impinged nerves with the goal of significantly reducing or eliminating pain.
While most traditional neck and back braces simply cinch tight around the patients’ torso to immobilize the area which can assist with the pain, DDS decompression braces (the 500 and Double back braces and MAX collar) target the cause of the pain. This happens when prolapsed, bulging or herniated discs are able to distract off impinged nerves and begin to rehydrate within their respective intervertebral disc spaces. The DDS 500, Double and MAX are constructed of dozens of vertical air chambers that expand vertically as they are inflated once the brace is on the patient. As they expand vertically they create lift against the torso thus stretching/decompressing/distracting the lower back.
The way to calculate the distractive force of a given DDS brace, simply multiply the psi the brace is inflated to with the total number of vertical air chambers found in the brace in question.
According to in-house testing conducted by the creators/engineers and manufacturers of the DDS 500, Double and MAX; when inflated to 14 psi, one air chamber in a DDS 500 back brace creates 2.7 lbs of distraction force and 3.6 lbs of distraction force in the Double brace. In the MAX cervical collar one air chamber creates about 3 lbs of distraction force. Using these numbers multiplied by the number of vertical air chambers in the various sizes of each brace, the DDS 500 can create from just shy of 61 lbs to just under 111 lbs of distraction force. The Double can create from 68.78 lbs to 133.94 lbs, and the DDS MAX (which is a one-size-fits-all device) has a distractive force of 24.32 lbs.
DISTRACTIVE FORCE CHART
The chart below illustrates exactly much distractive force each brace type produces in each size.
| LBS PER CHAMBER | Number of Chambers | Distractive force (LBS) | |
|---|---|---|---|
| ONE SIZE FITS MOST | X | X | X |
| S | 2.77 | 22 | 60.94 |
| M | 2.77 | 25 | 69.25 |
| L | 2.77 | 28 | 77.56 |
| XL | 2.77 | 31 | 85.87 |
| 2XL | 2.77 | 34 | 94.18 |
| 3XL | 2.77 | 37 | 102.49 |
| 4XL | 2.77 | 40 | 110.80 |
| 5XL | 2.77 | 40 | 110.80 |
| 6XL | 2.77 | 40 | 110.80 |
| 7XL | 2.77 | 40 | 110.80 |
| LBS PER CHAMBER | Number of Chambers | Distractive force (LBS) | |
|---|---|---|---|
| ONE SIZE FITS MOST | X | X | X |
| S | 3.62 | 19 | 68.78 |
| M | 3.62 | 22 | 79.64 |
| L | 3.62 | 25 | 90.50 |
| XL | 3.62 | 28 | 101.36 |
| 2XL | 3.62 | 31 | 112.22 |
| 3XL | 3.62 | 34 | 123.08 |
| 4XL | 3.62 | 37 | 133.94 |
| 5XL | 3.62 | 37 | 133.94 |
| LBS PER CHAMBER | Number of Chambers | Distractive force (LBS) | |
|---|---|---|---|
| ONE SIZE FITS MOST | 3.04 | 8 | 24.32 |
Dr. Mark Baxter, a decompression physician who has been practicing in Las Vegas, NV for over 20 years, explains that it has to do with the psi pressure the brace is inflated to times the square inches of contact surface along the upper edge of the brace that rests upon the patient's body and exerts an upwards force.
For example, the belt thickness of the DDS 500 is about ½ inch. For a brace suited on a patient with a 40-inch circumference there will be approximately 80 of these columns, each one of which is ¼ inch of a square inch. In this case, the math states that the contact surface area would total 20 square inches. Therefore the amount of force exerted on the patient's body would be 20 square inches times the psi the belt is inflated to (approximately 14 psi), which would total to 248 pounds of distractive lift.
Conclusion
When worn properly for the suggested amount of time, the distractive force of the DDS 500, Double and MAX are measurable and can have amazing effects on decompressing the cervical and lumbar region of the spine. This can lead to significant pain relief and the creation of an optimal healing environment in which damaged discs may rehydrate and recover.
ISOKINETIC EVALUATION
Supplement to the Air Brace Clinical Studies
Air Brace vs. Muscle Atrophy
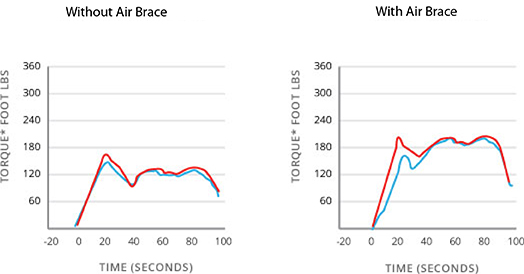
Lumbar Flexors
This graph illustrates that while wearing the Air Brace, the average sustained torque* of the lumbar flexor muscle is approx 180 torque* pounds compared to approx 130 torque* pounds without wearing the Air Brace
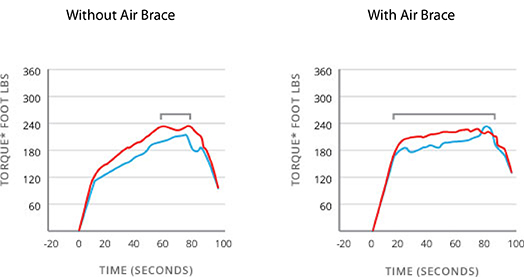
Lumbar Extensors
This graph illustrates that while wearing the Air Brace the lumbar extensor muscles reach maximum torque* faster and sustains maximum torque* 3 times longer.
Conclusion
The Air Brace promotes muscle stimulation and activity, which is in contrast to most other lumbar supports which limit mobility thus promoting muscle atrophy resulting in weakness of the lower back and dependency upon the brace.
Types of Spinal Diseases, Injuries and Back Pain
DDS Decompression Braces are the perfect tool to help those with the following indications. Our Decompression Braces, including the DDS 500 and DDS DOUBLE, have been proven to relieve pain, sometimes as quickly as within the first 20 minutes upon application. Spinal decompression is created as the brace is inflated. The vertical air cell expansion mechanism decreases the axial loading while increasing the intervertebral disc space by anchoring up underneath the rib cage pushing upwards, and down against the pelvic girdle pushing downwards. This action stretches the torso vertically, diverting the weight bearing forces away from the discs and reducing the pressure within the lumbar spine region, significantly reducing pain levels while assisting active-rehabilitation. The traction effect provides support to assist the weakened disc.
Spinal sprain (lumbar sprain)
Spinal (lumbar) sprain refers to the shock or damage of light muscle or ligament caused by lifting heavy objects, performing rigorous physical activity, excessive exercising or due to a traffic accident. You might have described or have heard someone else describe this condition with this common phrase: “I pulled my back” or “I threw out my back.” A simple lumbar sprain can be alleviated by bed rest for a few days. However, a significant number of these cases can lead to the development of chronic backache or disease that affects everyday life. Although a sprain of the wrist or ankle can be treated by fixing the affected area with a cast or a wrap, the same can hardly be done for a spinal sprain. Once a patient begins to experience pain in the sprained area, the corresponding muscle and ligament stiffen up from this pain. One should limit their movements and apply hot and cold packs. Stretching can also be beneficial as well as taking anti-inflammatory medicine.
Herniation of Intervertebral Disc
We all have discs that act as cushions between our spinal bones. These discs are made up of an outer annulus fibrosus, which surrounds the inner nucleus pulposus. In one instance of a herniation of the intervertebral disc, there is a tear in the annulus fibrosis and the nucleus pulposis is no longer fully protected. Most of the time when the intervertebral disc is herniated it is titled to the left or right. When the herniation is to the left the pulp compresses the left side of the nerve generating pain on the left side of the lower body and does the same to the right when the herniation is to the right. Pain is not limited to the waist area, however. Frequently, there is accompanying pain in the sacrum, hips, posterior thigh, toes, etc. The pain is a result of inflammation and compression of the nerve. In the case of a bulging disc, the symptoms and treatments are very similar to those of a herniation of the intervertebral disc (herniation of vertebral pulp). However, the nerve is compressed not by a herniated pulp but by the protrusion of the entire disc itself.
Spinal Stenosis
Spinal Stenosis is a type of degenerative disease where there is a loss of moisture in the disc primarily due to aging. The loss of moisture causes decreased elasticity or internal deformity of the disc. Once the internal disc (pulp) is weakened, it will eventually collapse since it can no longer withstand the body weight. The narrowing of the intervertebral space caused by this collapse is called spinal stenosis. Many cases of chronic herniation of the intervertebral disc can lead to the development of spinal stenosis.
Spondylolysis & Spondylolisthesis
Spondylolysis is caused by a fracture or loss of the posterior joint connecting one vertebral bone to another. This is the most common cause of low back pain in adolescent athletes that can be seen on X-rays. This stress fracture in one of the bones (vertebrae) that make up the spinal column usually affects the fifth lumbar vertebra in the lower back and, much less commonly, the fourth lumbar vertebra. If the stress fracture weakens the bone so much that it is unable to maintain its proper position, the vertebra can start to shift out of place. This condition is called spondylolisthesis. If too much slippage occurs, the bones may begin to press on nerves and surgery may be necessary to correct the condition. There may be a hereditary aspect to spondylolysis. An individual may be born with a thin vertebral bone and therefore may be vulnerable to this condition. Significant periods of rapid growth may encourage slippage. In many people, spondylolysis and spondylolisthesis are present, but without any obvious symptoms. Pain usually spreads across the lower back and may feel like a muscle strain. Spondylolisthesis can cause spasms that stiffen the back and tighten the hamstring muscles, resulting in changes to posture and gait. If the slippage is significant, it may begin to compress the nerves and narrow the spinal canal. In most cases, strengthening and stretching of the back and abdominal muscles along with physical therapy and a back brace can help to prevent future occurrences of this painful condition.
Compression Fracture
The Vertebra is crushed and collapses from excessive pressure or trauma. Most healthy bones are able to withstand pressure and the spine is able to absorb the shock of trauma. However, if the force is too strong or the spine is very weak, a vertebra may fracture. Compression fractures are likely when the spine is bent forward at the same time there is downward pressure on impact such as a car accident or falling to the floor in a various positions.
Osteoporosis is often the underlying cause of compression fractures. Osteoporosis is usually caused by the aging process, which weakens and thins bones because of the loss of calcium and nutrients. When the vertebra becomes too weak to withstand normal pressure, additional pressure and trauma may cause it to collapse.
Symptoms can include severe pain in the back and legs. It can also cause numbness and weakness.
Degenerative Disc Disease
Degenerative Disc Disease is the degeneration, advanced aging or breaking down of an intervertebral disc of the spine. Findings show the narrowing of disc space between the vertebrae from the loss of fluid in the discs. It reduces flexibility and further reduces the ability for the discs to act as shock absorbers.
DDD may lead to a wide range of spinal diseases and injuries.
Muscle Spasms
Often called back spasm, spinal muscle spasms are spontaneous contractions of the muscles leading to back pain or sometimes the ability to move. It can be attributed to overuse or an injury and the onset is more common for those who have experienced it.
Generally, spasms are preceded by small strains leading to inflammation. Conditions such as degenerative disc disease and herniated disc may compress a nerve root causing irritation. The body attempts to immobilize the area to stop pain by tightening and contracting the muscles. Preventions include stretching, PT and exercise to strengthen the lower back muscles.
Sciatic Nerve Pain/ Radiating Pain
Sciatica is a symptom and not a diagnosis for a spinal injury. It is commonly associated with the above diagnoses. Pain is caused by a general compression or irritation of the sciatic nerve. Symptoms include lower back pain, buttock pain, numbness, a burning sensation, pain and weakness in the leg or foot. It can include “pins and needles” sensation or tingling in the leg. Specific sciatica symptoms can be different in location and severity. Treatment is focused on the underlying causes of symptoms.
Knee Pain and Arthritis in the Knee
Osteoarthritis
The knee is the largest and strongest joint in the body. It is made up of the femur/thighbone, the tibia/shinbone and the patella/ kneecap. Articular cartilage covers the ends of the three bones where they touch and it is a smooth, slippery cushioning substance that protects the joint as you bend and straighten the knee. Osteoarthritis is the condition in which the cartilage between the knee joints wears away. The femur and tibia bones rub more closely against one another causing pain, swelling, stiffness and limited mobility. The formation of bone spurs is also common. The chance of developing osteoarthritis rises after the age of 45 and its most common in women. The most common cause of OA of the knee is age. Other causes are weight gain, heredity, gender, repetitive stress injuries, athletics and other illnesses such as rheumatoid arthritis. Treatments include weight loss, exercise, medication, injections, PT and surgery. Bracing is used to help prevent less contact between the bones and helps increase mobility.
