100 Healthcare Stats from Becker’s Hospital Review
1. There are 5,723 hospitals in the U.S., according to the most recent American Hospital Association data available to the public.
2. There are 4,999 community hospitals in the U.S.
3. There are 1,326 critical access hospitals in the U.S., according to data from the Flex Monitoring Team.
4. Nonprofit hospitals spend the most on inpatient stays compared to other hospital ownership types, according to Kaiser State Health Facts. Hospital adjusted expenses per inpatient day by ownership is as follows:
– Nonprofit hospitals: $2,088
– State/local government hospitals: $1,667
– For-profit hospitals: $1,628
5. There are 893,851 professionally active physicians in the United States, according to Kaiser State Health Facts.1
6. Of the professionally active physicians in the country, 425,032 are primary care physicians and 468,819 are specialty physicians.1
7. Approximately 32 percent of physicians are women.1
8. There are 48,806 physicians specializing in surgery.1
9. There are 46,089 physicians specializing in anesthesiology.1
10. There are 45,140 physicians specializing in emergency medicine.1
11. There are 43,822 physicians specializing in radiology.1
12. There are 28,700 physicians specializing in cardiology.1
13. There are 16,217 physicians specializing in oncology.1
14. There are 6,546 physicians specializing in endocrinology, diabetes and metabolism.1
15. There are 50,416 physicians specializing in psychiatry.1
16. There are approximately 27,773 orthopedic surgeons in the United States, as of the 2012 Orthopaedic Surgeon Census by the American Academy of Orthopaedic Surgeons.
17. Across all specialties, approximately 21 percent of physicians are employed by a hospital.
18. The number of hospital medicine groups employing nurse practitioners and physician assistants has increased to 65.5 percent from 53.9 percent in 2012.
19. Family medicine is the most in-demand clinician specialty, according to a Merritt Hawkins report.
20. The United States is ranked 25th in regards to physician count per capita among international peers, with 2.5 physicians per 1,000 people, according to an Organization for Economic Cooperation and Development report.
21. By 2020, the U.S. is expected to be short more than 9,000 physicians and short 130,000 physicians by 2025, according to Association of Medical Colleges projections.
22. Sixty-seven percent of the 51.6 million hospital-based services in 2012 was provided by hospitalists as opposed to traditionalists (primary care physicians and others whose services primarily take place outside an acute-care facility), according to an analysis of Medicare payment data.
23. Physician assistants make up about 10 percent of the primary care workforce and represent 9 percent of clinicians in community health centers.
24. There are roughly 5,500 ambulatory surgical centers in the United States.
Hospital & Health System Compensation
25. Non-system hospital CEOs saw the largest base salary growth of all job categories at a 4.3 percent increase, according to the 2014 Hay Group Healthcare Compensation Study.
26. From January to July of 2014, less than half — 40 percent — of hospital C-suite hires were internal promotions, according to a Billian’s HealthDATA report.
27. Since 2012, the median salary for non-academic adult hospitalists has increased 8.2 percent annually, from $233,855 to $252,996, according to the Society of Hospital Medicine’s 2014 State of Hospital Medicine report.
28. Hospitalists at non-academic pediatric hospitals saw a median compensation increase of 9.5 percent, from $178,885 to $195,832, over the past two years.
29. On average, physician and surgeons earn a national estimated wage of $191,880, according to the Bureau of Labor Statistics.
30. Registered nurses earn an average national estimated wage of $68,910.
31. Nurse practitioners earn an average national estimated wage of $95,070.
Health Coverage
32. Roughly 10.3 million adults in America gained health coverage between January 2012 and June 2014, according to a study published in The New England Journal of Medicine.
33. The number of uninsured Americans dropped by 3.8 million from January to March, which brought the average percentage of people without health insurance to 13.1 percent, according to a survey by the Centers for Disease Control and Prevention’s National Center for Health Statistics.
34. On average, healthcare cost nearly $9,000 per person in 2012, according to the Bureau of Labor Statistics.
35. On average, healthcare for a typical family of four covered by an employer-sponsored preferred provider organization plan currently costs roughly $23,215. That cost is nearly twice what it was a decade ago but the year-over-year increase of 5.4 percent between 2013 and 2014 is the lowest growth rate recorded by the Milliman Medical Index since it was first calculated in 2002.
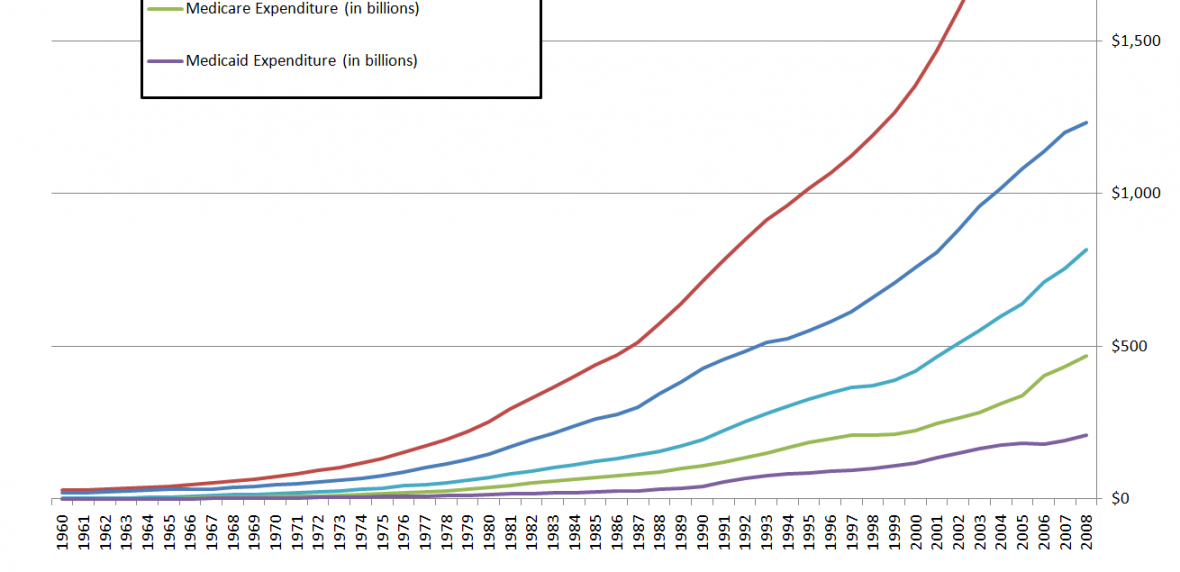
36. National healthcare spending is projected by CMS to increase 4.7 percent from 2013 to 2015.
Medicaid
37. As of Aug. 28, 28 states (including Washington, D.C.) have expanded Medicaid coverage, two states are in debate over the implementation of coverage expansion and 21 states are not moving forward with the decision at this time.
38. As of Aug. 28, there are approximately 14,466,000 uninsured adults and children living in the U.S. who are eligible for Medicaid under the Patient Protection and Affordable Care Act, according to Kaiser State Health Facts.
39. Also as of Aug. 28, there are roughly 4,524,090 poor uninsured non-elderly adults that fall within the PPACA coverage gap, according to Kaiser State Health Facts.
40. The number of uninsured patients seeking treatment from safety net hospitals is expected to drop to 13 million people this year due to the expansion of insurance.
41. Projections estimate Medicaid spending will increase 12.8 percent and private health insurance spending will increase 6.8 percent in 2014 due to the availability of more coverage options on the insurance marketplaces, according to a CMS report.
42. In 2012, Medicaid costs totaled $432 billion, of which the non-federal share was about $180 billion.
43. States across the nation have increasingly relied on healthcare providers and local governments to finance the non-federal portion of Medicaid payments, rising by more than 21 percent from state fiscal year 2008 through 2012, according to a report from the Government Accountability Office.
44. Health centers in states that didn’t extend Medicaid gave up a combined total of $569 million in federal funding in 2014, according to a report from The George Washington University.
45. Hospitals in states that expanded Medicaid coverage provided about $1.9 million in charity care during the first quarter of this 2014, 32 percent less than the $2.8 million of charity care spent during the same time frame in 2013, according to a report from the Colorado Hospital Association.2
46. Hospitals in states that did not expanded Medicaid coverage provided about $4.2 million in charity care during the first quarter of this 2014, 11 percent more than the $3.8 million of charity care spent during the same time frame in 2013.2
47. In expansion states, self-pay charges dropped from 4.7 percent of all charges in the first quarter of 2013 to 3.1 percent during the first three months of this year.2
48. In the non-expansion states, self-pay charges rose slightly year-over-year during the first quarter, from 4.8 percent in 2013 to 5 percent this year.2
Medicare
49. The Congressional Budget Office projects Medicare is spending approximately $11,328 per person in 2014.
50. Medicare spending on outpatient hospital care has increased 126 percent from 2003 to 2012, according to the June 2014 Data Book of Health Care Spending and the Medicare Program.
51. CMS projections estimate Medicare spending will grow 7.4 percent annually from 2015 to 2022.
52. Medicare spent as much as $8.5 billion (2.7 percent of total spending) on services deemed to have little or no clinical value in 2009, according to a 2014 JAMA Internal Medicine study.
53. Approximately 3,400 acute-care hospitals and 435 long-term care hospitals receive payments under CMS’ Inpatient Prospective Payment System.
54. More than 4,000 hospitals and 5,300 Medicare-certified ASCs receive reimbursement through Medicare’s Outpatient Prospective Payment system.
55. Beneficiaries’ coinsurance accounted for approximately $1.5 billion — 47 percent — of the reimbursements for outpatient services provided in 2012 that CAHs received, according to an HHS Office of Inspector General report. Coinsurance rates for Medicare beneficiaries accounted for an average of 22 percent of the OPPS rates for outpatient services at acute-care hospitals.
56. CMS’ Open Payments website unveiled roughly 4.4 million payments were made to physicians and teaching hospitals from drug, medical device and biologics companies from August to December 2013, equaling approximately $3.5 billion.
57. Medicare penalized a record 2,610 hospitals this year under the Hospital Re-admissions Reduction Program for high readmission rates. Together, the total fines added up to roughly $428 million.
Hospital Construction
58. In the U.S., there are 37 relatively “firm” planned hospital construction projects that are estimated to cost $50 million or more, each, according to a report by Reed Construction Data.
59. Fifty-eight percent of the upcoming projects valued at $50 million or more each are considered new work, as opposed to hospital additions or alterations.
60. BJC Healthcare, a nonprofit organization based in St. Louis, is planning the largest dollar allocation for hospital construction in the country at $1.5 billion. The money will be dispersed in several St. Louis locations.
Accountable Care Organizations
61. As of May, the number of accountable care organizations in the United States exceeds 600, according to a May 2014 analysis from Leavitt Partners.
62. Approximately 20.5 million people are covered by ACOs, as of June, including the 5.3 million patients enrolled in the Medicare Shared Savings and Pioneer Programs.
63. Medicare ACOs represent roughly 60 percent of all ACOs in the country, according to CMS.
64. In a survey of 1,183 physician practices, 35 percent had already joined an ACO or planned to join one soon, while 60 percent had not joined an ACO and had no plans of joining one, according to a March 2014 study published in Health Services Research.
65. CMS and HHS estimated ACOs will save the Medicare program up to $940 million in the first four years.
66. There are 37 quality measures ACOs must meet to qualify for shared savings.
67. The Houston-based Memorial Hermann ACO had the most shared savings in performance year one of the Medicare Shared Savings Program, saving $28.34 million.
68. As of April, 19 states have moved toward the formation of Medicaid ACOs, including Alabama, Arkansas, California, Colorado, Connecticut, Hawaii, Illinois, Iowa, Maine, Massachusetts, Minnesota, New Jersey, New York, North Carolina, Oregon, Texas, Utah, Vermont and Washington.
69. Oregon leads in Medicaid ACOs with a total of 16 Coordinated Care Organizations covering more than 750,000 lives, according to Leavitt Partners.
70. As of April 2014, more than two-thirds of Americans live in areas served by an ACO and more than 40 percent live in areas served by two or more ACOs, according to an Oliver Wyman report.
Health IT
71. The Council for Affordable Quality Healthcare estimates the healthcare industry can save about $8.1 billion annually, including $6.7 billion in savings for healthcare providers and $1.4 billion for health plans each year, through additional conversions from manual to electronic transactions.
72. In 2012, paper-based claims submissions cost the healthcare system $2.58 each while electronic claims submissions only cost the healthcare system $0.54 each.
73. In 2013, 59 percent of non-federal acute-care hospitals in the U.S. had adopted at least a basic EHR system, according to the ONC, a 34 percent increase over 2012.
74. A majority of physicians — 83 percent — report they are using EHRs, according to a Medscape survey.
75. Since 2011, CMS has paid out almost $25 billion in incentive payments for the adoption and use of EHRs to hospitals and physicians.
76. By 2013, 89 percent of critical access hospitals had installed full or partial EHRs, although many CAHs did not meet the meaningful use criteria.
77. The EHR market is estimated to reach $9.3 billion annually by the end of 2015, and will likely continue to grow until at least 2018, according to a report from Kalorama Information.
78. The number of jobs for EHR technicians is expected to grow 22 percent, from 186,300 to 227,400 positions, between 2012 and 2022, according to a report from the U.S. Department of Labor.
79. A recent survey found a majority of patients — 83 percent — expect hospitals to use EHRs, but only 53 percent said they trust the safety and security of the software.
80. The global mHealth market is expected to be worth approximately $49.1 billion by the year 2020.
81. The global mHealth market is estimated to grow at a compound annual growth rate of 49.7 percent over the next six years.
82. Nearly half of physicians — 48 percent — used mHealth to determine medication interactions, followed by 27 percent for diagnosis tools and 19 percent to access EHRs, according to a MedData group study.
83. More than one-third of physicians have reported recommending an mHealth app to patients within the last year, and 47 percent have used their own devices to show patients images, according to a Manhattan Research survey.
84. Almost two-thirds, 65 percent of the nurses, said they use a mobile devices, social media and online references for professional purposes, according to a Wolters Kluwer Health survey analysis.
85. Nearly 75 percent of adults do not use any mHealth apps and fitness tracking devices, according to a Technology Advice survey of more than 900 adults.
86. Out of 600 of the most commonly used mHealth apps, less than one-third (30.5 percent) have a privacy policy, according to a study in the Journal of American Medical Informatics Association.
87. Only 100 of the approximately 100,000 mHealth apps available — or 0.1 percent — are FDA-approved, according to a report in the New England Journal of Medicine.
88. The largest data breach in 2014 so far compromised Franklin, Tenn.-based Community Health Systems security and has affected roughly 4.5 million people.
Patient Care and Quality
89. Roughly $4.1 billion in healthcare costs has been saved by hospitals’ improvements in patient safety, according to an HHS data report.
90. One-day prevalence surveys conducted between May and September in 183 hospitals of 11,282 patients revealed that 49.9 percent were on at least one antimicrobial drug, according to a report published in the Journal of the American Medical Association.
91. More than 11 million antibiotic prescriptions written for children each year may actually be unnecessary, according to a study in Pediatrics.
92. A majority of hospitals — 78 percent — have evidence of unnecessary antibiotic combinations being administered for two or more days, resulting in potentially avoidable healthcare costs of nearly $13 million, according to research conducted by the Centers for Disease Control and Prevention and Premier.
93. Of 63,418 total prescribed antibiotics, 7,876 (12.4 percent) were prescribed over the phone, according to a study in Pharmacoepidemiology and Drug Safety. Additionally, the rate of telephone-based prescribing increased over the study period from 2.2 prescriptions per 100 patient-years to 4.2 prescriptions per patient years.
94. Prescription drug spending is expected to account for approximately $272.1 billion of health expenditures in 2013 and increase 6.8 percent in 2014, according to a CMS report.
95. Pneumonia is the most common of all healthcare-associated infections, with a 21.8 percent prevalence, according to a survey published in The New England Journal of Medicine.
96. Every year, approximately one in 20 Americans, or about 12 million people, receiving outpatient care are misdiagnosed, according to a new survey by SERMO.
Miscellaneous Healthcare Statistics
97. Between 2009 and 2020, healthcare spending on mental and substance abuse disorders is expected to fall from 7.4 percent to 6.5 percent, according to a study from Truven Health Analytics.
98. From 2009 through 2020, patent loss will allow generic products with prices assumed to be about 70 percent lower than the price of the brand-name equivalents to enter into the market.
99. The average amount of time patients spent in the emergency department before being admitted to the hospital as an inpatient is 274 minutes, according to HHS Hospital Compare data.
100. On average, 71 percent of patients said, yes, they would definitely recommend the hospital they attended to friends and family.
Footnotes:
1 Kaiser State Health Facts, 2014.
2 Colorado Hospital Association, Center for Health Information and Data Analytics. “Impact of Medicaid Expansion on Hospital Volumes.” June 2014. Available online at http://www.cha.com/Documents/Press-Releases/CHA-Medicaid-Expansion-Study-June-2014.aspx
Editor’s Note: A previous version of the article ran that failed to mention that 5.4 percent growth between 2013 and 2014 was the lowest growth rate recorded by the Milliman Medical Index since 2002. The omission has since been remedied.
888-495-7440